Filling a Prescription for an Exceptional Access Drug
Prescriptions for an exceptional access drug can be flagged as EAP Drugs to indicate authorization for ODB coverage for a drug not listed as a benefit under the program (non-formulary). By overriding the drug’s eligibility for coverage, EAP Drugs prescriptions are flagged and sent as an online Drug Benefit claim.
To fill a new prescription for an exceptional access drug in PharmaClik Rx:
- Create a new prescription until you reach the Rx Detail stage.
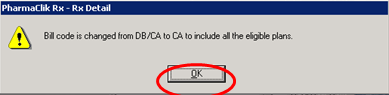
- The PharmaClik Rx - Rx Detail Warning indicates that the bill code DB (Drug Benefit) will be removed from the Bill field and displays this message because PharmaClik Rx recognizes the drug selected as a non-formularly benefit.
- Select OK to proceed.
- Select the Extended tab.
- Select the Eligibility Override checkbox to notify the system that the drug selected is eligible for the Drug Benefit (DB) program and to submit for adjudication. The PharmaClik Rx - Rx Detail warning displays.
- Select OK to proceed.
- Select the EAP Drugs checkbox.
- Select the Fill button.
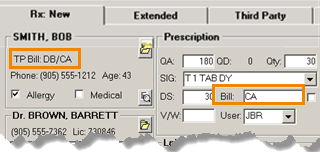
Result: The TP Bill code field displays DB/CA, indicating that the patient has Drug Benefit (DB) coverage and the Bill field displays only CA to indicate that the prescription will not be submitted for adjudication due to its non-formulary status.